Finding a path to improve Indigenous workforce and healthcare outcomes

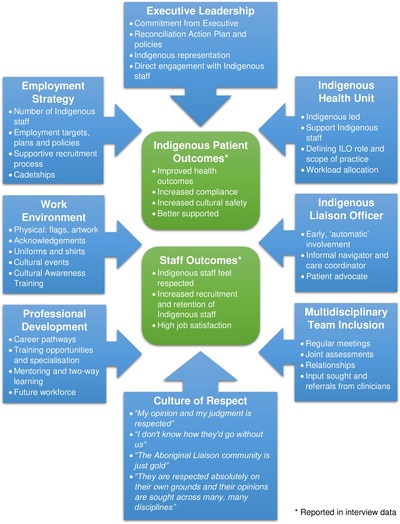
A study of two exemplary cancer services has found eight key factors helping to improve Indigenous patient and staff outcomes.
The study — a component of research within the DISCOVER-TT* CRE and published in PLOS ONE — investigated Indigenous workforce policies and strategies at two high-performing Australian health services (the Urban Service and the Regional Service) to inform innovative services for Indigenous cancer patients and their families. The services were identified in a national study as particularly high performing in their provision of cancer services for Indigenous cancer patients and their families.
In-depth interviews of Indigenous and non-Indigenous hospital staff, Indigenous cancer patients and their family members revealed eight core themes successfully supporting the Indigenous workforce:
- Strong executive leadership.
- A proactive employment strategy.
- The existence of an Indigenous Health Unit.
- The role of the Indigenous Liaison Office (ILO).
- Multidisciplinary team inclusion, including ILO participation.
- Availability of professional development.
- A supportive work environment.
- A culture of respect.
Improved Indigenous patient outcomes and improved Indigenous staff outcomes were reported where these eight factors were implemented.
“Many health services report difficulties recruiting and retaining Aboriginal and Torres Strait Islander staff. But we know that Indigenous staff improve outcomes for Indigenous patients as well as providing support for non-Indigenous staff,” said lead author Emma Taylor from the Western Australian Centre for Rural Health (WACRH) at the University of Western Australia.
“These exemplary cancer services and their affiliated hospitals show how positive patient outcomes and a strong Indigenous health workforce can be achieved when a health service has strong leadership, commits to an inclusive and enabling culture, facilitates two-way learning and develops specific support structures appropriate for Indigenous staff,” the authors wrote.
“It is hoped that the strategies captured in this study will be used by health services and cancer services to inform their own policies and programs to support building their Indigenous workforce.”
The authors explained that although many Aboriginal and Torres Strait Islander people enjoy good health, health outcomes between Indigenous and non-Indigenous Australians remain disparate across a wide range of diseases, including cancer. They also highlighted that, despite reductions in the Indigenous mortality rate from chronic diseases, the gap in cancer mortality rates is widening.
Executive leadership
The researchers noted that the executive team at both health services had a strong commitment to improving Indigenous health outcomes, strengthening the cultural safety of their services and to supporting and growing their Indigenous workforce. Both services have made commitments to improving Indigenous health on their strategic plans and both actively implement their hospital’s Reconciliation Action Plan (RAP).
Employment strategy
Compared with most other hospitals included in the initial survey of cancer services, the two high-performing services employ a large number of Indigenous staff, with some working in identified Indigenous roles.
As at February 2020, the Urban Service employed 52 Indigenous staff (0.9% of the total workforce) and the Regional Service employed 241 Indigenous staff (3.7% of the total workforce). Both services have specific and measurable targets set for the employment of Indigenous staff. In addition, the Urban Service has recently implemented a cultural leave policy, which provides Indigenous staff with access to four days’ cultural and ceremonial leave.
ILOs are valued and respected team members
Both health services have an Indigenous-led Indigenous Health Unit, which is responsible for managing the ILOs, supporting Indigenous staff, designing and delivering cultural awareness training and quality improvement. Significantly, both of the units feel that they are afforded enough autonomy and independence to ensure that what they do is Indigenous led.
The services operate centrally managed Indigenous teams, with the unit providing managerial and cultural support for staff, as well as Indigenous colleagues with whom they can network and debrief, and allowing for work to be allocated across the team, which helps prevent staff from being overworked.
Within these services, the ILO role is a valued and respected role within the multidisciplinary team and is seen as a linchpin that helps to coordinate care and ‘join the dots’ between patients, their families, staff and the community. The ILO is described as having ‘automatic’ involvement with any Indigenous patient, acting as an advocate to ensure their wishes are communicated and upheld. System functionality helps with workload allocation and ensures that no patients are missed.
One patient commented, “I have really appreciated the support I’ve received from the Aboriginal liaison officer… they have gone above and beyond what they have to do just to make sure I’m right. Without their support I don’t know where and what head space I would be in. I probably wouldn’t even still be in hospital. They have done all they can to keep me here and, yeah, I probably would have done a runner and gone back to [town] by now if it wasn’t for their support and understanding.”
ILOs bring a cultural safety component to care situations and are consulted by doctors and other healthcare staff when discussing patients.
Managers and patients at the Urban Service said that ILOs increased treatment compliance and reduced the rate of discharge against medical advice.
Indigenous staff increased the cultural safety within the facilities through their presence and interactions with patients, but also through advising non-Indigenous staff.
Professional development and two-way learning is encouraged
The study authors wrote that, “Career development for Indigenous staff was an action item on both Reconciliation Action Plans, with one service aiming to develop career pathways and the other service targeting 100% of all Indigenous staff to develop a career plan with their manager as part of their annual performance plan.”
Indigenous staff at the two services are supported to achieve higher qualifications, and ILOs are encouraged to specialise in a particular therapy area to build upon their expertise and help patients with specific needs.
Informal mentoring, clinical placements and specific mentoring for Indigenous students studying medicine, nursing and allied health are also important aspects of staff development.
The Urban Service has established an Indigenous Cadetship Program as well as a Graduate Nursing Program that sits within the Indigenous Health Unit to ensure a culturally safe entry point into the program.
An Indigenous Manager explained, “The idea is to bring Aboriginal students in and give them exposure working in a hospital environment in order to better prepare them for the workplace.
“We are hopeful these cadets come back to us through the graduate nursing program and build a career here. We want to give them exposures so they know what to expect.”
Culturally safe and respectful work environment
The two services described in the research paper have made significant efforts to develop a culturally safe working environment, with physical representations of respect — including displaying the Aboriginal and Torres Strait Islander flags and artwork created by local Indigenous artists — throughout both hospitals. Acknowledgement of Country is clearly displayed at service entrances and features in all meetings; ILOs have their own uniform to legitimise the role and make them easily identifiable to staff and patients.
Staff are encouraged to participate in events such as Reconciliation Week and NAIDOC week to remove barriers to staff attending cultural events.
Cultural awareness training allows non-Indigenous staff to increase their knowledge and understanding of Indigenous cultures, history and achievements.
“The deep respect felt for Indigenous staff at these services came through strongly in every interview,” noted the researchers. This was observed at all levels of the organisations and contributed to Indigenous staff feeling respected and supported.
Indigenous staff outcomes
The health services reported good staff recruitment and retention rates, with each having several long-term Indigenous employees. Indigenous staff members reported feeling satisfied with their jobs as a result of being able to improve outcomes for their community. Non-Indigenous staff recognised the benefits they received from working closely with their Indigenous colleagues in terms of patient outcomes, team morale and improving their understanding of Indigenous Australians and their culture.
Both services are continuing to make improvements and are committed to closing the gap in health outcomes between Indigenous and non-Indigenous Australians.
Remote laundries target preventable disease in NT communities
A new community laundry has launched in Borroloola, part of a program seeking to curb preventable...
Eye care partnership looks to support First Nations optometrists
A new scholarship initiative will support Aboriginal and/or Torres Strait Islander optometrists...
A Day in the Life of a mobile optometrist
Linda Nguyen is the owner and founder of mobile optometrist practice Care Optometry and was a...

![[New Zealand] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89856/wfmedia_thumb/..jpg)
![[Australia] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89855/wfmedia_thumb/..jpg)




