Dramatic increase in cardiac implants
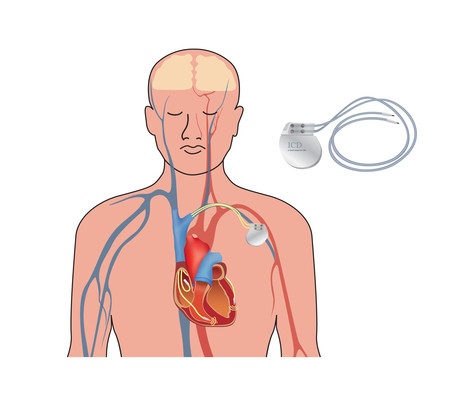
There has been a dramatic increase in the number of implantable cardioverter defibrillators (ICDs) inserted in patients over the past decade, at a cost of almost $155 million a year. More than 75% of procedures were in men.
A new Australian study has analysed the data from the National Hospital Morbidity Database to determine the number of ICD procedures by year, patient age and sex, and to estimate age group-specific population rates and associated costs.
The researchers, led by Dr Jodie Ingles, Head of the Clinical Cardiac Genetics Group at the Centenary Institute, found that the number of ICD procedures increased from 1844 in 2002–03 to 6504 in 2014–15.
“In 2014–15, the ICD insertion rate for people aged 70 or more was 78.1 per 100,000 population, 22 per 100,000 for those aged 35–69 years, and 1.40 per 100,000 people under 35,” Ingles and colleagues wrote.
“The reported complication rate decreased from 45% in 2002–03 to 19% in 2014–15, partly because of a change in the coding of complications [from ‘severe and catastrophic’ to ‘catastrophic’ only]. The number of removals corresponded to at least 4% of the number of insertions each year.
“The aggregate cost of hospitalisations with an ICD procedure during 2011–14 was $445,644,566.
In terms of specific ICD procedures, the authors found:
- The rate of ICD insertion procedures increased from 5.68 in 2002–03 to 17.9 per 100,000 persons in 2014–15.
- The rate of ICD replacement procedures increased from 1.67 in 2002–03 to 8.55 per 100,000 persons in 2014–15.
- The rate of ICD adjustment procedures increased from 0.23 in 2002–03 to 0.46 per 100,000 persons in 2014–15.
- The rate of ICD removal procedures increased from 0.27 in 2002–03 to 0.77 per 100,000 persons in 2014–15.
“It is unclear whether the overall increase in procedure rates reflected an increasing need for ICD therapy, or was a direct result of increased awareness of risk factors for sudden death,” Ingles and colleagues wrote.
“A patient-centred approach to care, including discussing the benefits and risks of ICD therapy with the patient and their family, is essential. The proportion of women among patients undergoing ICD procedures is relatively small (about 20%); the possibility that ICD therapy is underused in female patients should be investigated.”
The authors were surprised by one set of results in particular — the increased rate of ICD removals. “The most frequent reasons for ICD removal are post-surgical infection (clinically accepted infection rate: 1%), device malfunction, misdiagnosis of a heart condition, or lack of clinical benefit,” they wrote.
“The unexpectedly high rate of removals we found should be a priority for investigation.”
The research has been published in the Medical Journal of Australia.
$1bn vaccine and antivenom manufacturing facility opens
A $1 billion cell-based influenza vaccine and antivenom manufacturing facility has opened in...
National concussion clinical guidelines now available
The first Australia- and New Zealand-specific guidelines for all forms of concussion — from...
Doctors criticise "risky prescribing agenda"
The AMA and RACGP have expressed disappointment in the Pharmacy Board of Australia's...




![[New Zealand] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89856/wfmedia_thumb/..jpg)
![[Australia] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89855/wfmedia_thumb/..jpg)



