Ultrasound - The quiet achiever in medical imaging
Thursday, 25 July, 2013
Ultrasound is the quiet achiever in available medical imaging modalities, enabling a substantial and unique picture of the patient, writes Dr Matthew Andrews FRANZCR, past President of the Royal Australian and New Zealand College of Radiologists (RANZCR) and the Australasian Society of Ultrasound in Medicine (ASUM).

The RANZCR counters that no matter how technologically exquisite the images are,they are still no substitute for the ability to assess the patient in ability to assess the patient in conjunction with the ultrasound.”
“The ability to see inside the living human body has revolutionised medical practice over the last century, commencing with the discovery of x-rays and continuing with ever-sophisticated methods of not only looking at static structures, but observing and quantifying function at microscopic and biochemical levels.
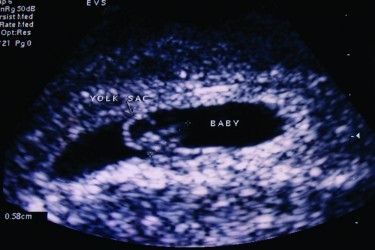
Ultrasound is one of the many available imaging modalities, enabling a substantial and unique picture of the patient. Many people are familiar with its use in obstetrics, where foetal viability, dates and anomalies are determined, but there is an ever-expanding range of medical ultrasound applications.
The simple principle of ultrasound is that high frequency sound waves, outside the human audible spectrum are transmitted through tissue. Differing proportions of the sound are either transmitted or reflected depending on particular tissue characteristics. The ratio of transmission: reflection is unique to tissue types, allowing a visual representation to be constructed.
Further advances have enabled assessment of blood flow (Doppler). Ultrasound is viewed in “real-time” allowing assessment of body function such a heart movement, blood flow and muscle and tendon movement. More recently 3D and 4D (moving3D) ultrasound clinical applications have been developed, providing even more life-like representation.
Paralleling and facilitating the proliferation of ultrasound applications, the machines have advanced becoming more compact and portable, simpler to operate and provide ever improving images. Reduction in machine prices has made ultrasound more affordable to a wide range of medical practitioners.
There are few areas in medicine which do not use some form of imaging. Options include x-rays CT, MRI, nuclear medicine and ultrasound. When a patient requires imaging for a particular clinical condition, it is vital that the most appropriate modalities are utilised. Criteria include the efficacy, availability, cost and radiation dose. A key role of the radiologist is to determine the appropriate imaging. If it can provide the clinical answer, ultrasound should be one of the first options, having the advantages of no radiation, low cost and ability to image in real time.
Ultrasound also plays a key role in interventional procedures. Its real time capacity allows direct visualisation of needle tip placement in the body, which is the common first step of many interventional procedures such as biopsies, drainages, stent placement.
Unfortunately, ultrasound does have limitations and disadvantages. Because ultrasound waves cannot penetrate air or bone, ultrasound is of little value in visualising the skeleton and lungs. Ultrasound is also operator-dependent meaning that images produced are not standardised as with other modalities such as CT or MRI. Unless the machine operator actually sees and records an abnormality whilst scanning, then independent review of images is of limited value. This partly accounts for it becoming so popular in the clinical or point of care situation, because the operator is the managing a clinician who can act directly on his/her ultrasound findings.
Ultrasound Providers
Medical ultrasound is performed under a range of service models. In Australia, radiologists form the medical group providing the largest proportion of ultrasound services on a referred basis. They are trained in ultrasound scanning and interpretation as part of their medical imaging specialty, which covers all imaging modalities. Nowadays, most radiologists do not perform the scans. These are done by sonographers, highly skilled technologists who together with radiologists work as a team to optimise scanning technique and medical imaging specialist expertise in the interpretation, correlation with other imaging.
The referred ultrasound service of this model is where the patient’s managing clinician referrers the patient to a radiologist for an ultrasound. The radiologist provides images and an ultrasound report; a medical specialist opinion, based on the ultrasound study. Referred ultrasound services may also be provided by sonologists (medical specialists with ultrasound expertise) with backgrounds other than radiology. These include obstetricians, vascular surgeons and cardiologists. They usually provide ultrasound related to their medical specialty.
The other distinct model of ultrasound service is “clinician-performed” or “point of care (POC)” ultrasound. Here it is used by the clinician as a clinical tool, where it often described as the electronic stethoscope, to extend and facilitate the clinical examination of the patient. Such applications are rapidly expanding and are also driven by the ultrasound machine price reduction, user friendliness and portability. These studies are usually limited in coverage, do not involve a sonographer or production of an ultrasound report and images are usually not recorded. Clinicians increasingly use ultrasound to guide procedures such as joint or tendon sheath injections, biopsies, vascular procedures and intraoperatively.
Of all areas of medical imaging, ultrasound has the widest range of providers. On some levels, this has lead to it being highly political, resulting in turf battles, with considerable differences in who should perform it and how it should be performed. On other levels, it has become a focus of great professional collaboration between the many groups involved, manifest by the membership of the Australasian Society of Ultrasound in Medicine (ASUM), which brings a range of medical practitioners, sonographers, scientists and the trade together to advance ultrasound practice in united approach.
Ultrasound Supervision
So-called ultrasound “Professional Supervision” is one of the more contentious issues in ultrasound practice. Professional Supervision has been defined as the medical input into the ultrasound examination, when a sonographer scans the patient. It has been derived, because the sonologist is ultimately responsible for the conduct of the examination.It is an unfortunate and inappropriate term implying that the sonologist is the only professional involved, whereas both members of the team are clearly professionals collaborating to add their individual expertise and experience to achieve the optimal result.
Delivery of supervision causes major differences amongst ultrasound players. The Royal Australian and New Zealand College of Radiologists (RANZCR)’s position is that the “supervising” sonologist should be physically present at the site of the study, so that when necessary he/she can medically assess the patient in the context of the ultrasound findings. Part of this may involve direct scanning, being present whilst the sonographer scans or directed physical examination of the patient.
The rationale is that because ultrasound is a dynamic modality, with non standardised images, the sonologist’s medical specialist expertise adds to the study. In some cases, this can only be maximised by directly assessing the patient. Others argue that ultrasound can still be supervised, even if the sonologist is off-site particularly with the use of tele-ultrasound where images can be viewed remotely. The RANZCR counters that no matter how technologically exquisite the images are, they are still no substitute for the ability to assess the patient in conjunction with the ultrasound.
The debate is further clouded by the recognition that certain types of ultrasound studies are more routine and technologically based (such as the assessment of vascular structures), whereas others such as musculoskeletal ultrasound frequently benefit from direct sonologist input. Patient’s presenting with conditions such as unknown abdominal or pelvic pain are also better assessed if the sonologist can combine ultrasound with a limited physical examination, which can only occur if the sonologist is on site.
Medical Ultrasound Training
Sonologists have dedicated medical specialist qualifications in ultrasound. Radiologists receive their qualification as part of the radiology fellowship. The most frequently obtained qualifications gained by non-radiologist specialists are the Diploma of Diagnostic Ultrasound (DDU) and the Certificate of Obstetric and Gynaecological Ultrasound (COGU).
Point of care ultrasound qualifications are in evolution and are complex due to the wide range different applications across the clinical spectrum, yet most clinicians use ultrasound in a limited manner pertaining to their scope of medical practice. The Australasian Society of Ultrasound in Medicine (ASUM) has established the Certificate of Clinician Performed Ultrasound (CCPU) in several clinical disciplines initially including emergency medicine, anaesthetics, obstetrics and gynaecology and neonatal medicine. Many other CCPU subgroups will emerge in the future.
Amazingly, Medicare currently pays ultrasound rebates without a specific medical ultrasound qualification.RANZCR and other interested groups have lobbied without success to have this anomaly addressed.
Sonographer Training
For an ultrasound service in which a sonographer has been used, Medicare provide a rebate only if the sonographer is accredited.An appropriates qualification, either a degree or diploma are components for accreditation with the Australian Sonography Accreditation Registry (ASAR).
Safety
Ultrasound uses no ionising radiation and there are, to date, no demonstrated adverse biological effects of ultrasound.This does not mean that ultrasound is necessarily safe. Ultrasound expert organisations, such as RANZCR, RANZCOG and ASUM recommend ultrasound exposure should be limited to what’s needed to provided the necessary diagnosis, especially with early pregnancy ultrasound during embryonal organogenesis.
The ALARA principle (ie the ultrasound needed to provide the diagnosis should be As Low As Reasonably Achievable) of radiation dose should also apply to ultrasound, even though there is no currently demonstrable adverse effect. Doppler studies use the highest amount of ultrasound energy which manifests as heat gain in tissue. The prudent use of Doppler ultrasound in early pregnancy is thus recommended.
Entertainment Ultrasound
The life-like foetal images produced by state of the art ultrasound machine have spawned an ultrasound entertainment industry, offering non-diagnostic “pictures of your baby”. These are often performed by non-qualified operators. RANZCR, RANZCOG, ASUM and other ultrasound organisations all oppose this non-medical use of ultrasound mainly on the grounds of potential harm to the foetus.
Funding
Whilst ultrasound is a relatively inexpensive imaging modality, it accounts for a large and growing proportion the diagnostic imaging outlays by Medicare. In 2011/12, Medicare funded just over 7.3 million ultrasound services, accounting for 36 per cent of private diagnostic imaging services. d just over 7.3 million ultrasound services, accounting for 36 per cent of private diagnostic imaging services. Medicare has a responsibility to ensure services it pays for are clinically appropriate and are funded properly. It should only pay for ultrasound studies provided by ultrasound-qualified medical practitioners.
With the development of two distinct streams of ultrasound, the RANZCR believes the current model of ultrasound payment should be reviewed. Referred and Point of Care ultrasound have significantly different cost components and thus should be remunerated differently. As POC ultrasound is a component of the clinical examination, the RANZCR believes it should be paid as such. The referred ultrasound usually involves a high-end (more expensive) machine, has images obtained by a sonographer, which are provided to the patient and archived and the issuing of a report. Its cost inputs are thus greater.
Future Trends
Ultrasound will remain a major component of medical imaging, with further streaming into the two major streams of referred and clinician performed ultrasound. Because ultrasound is deemed safe,the temptation is to overuse it.
Any imaging test, including ultrasound should only be used if it is appropriate for the clinical condition and the test improves patient outcome. It is very likely that currently a significant proportion outcome. It is very likely that currently a significant proportion of ultrasound studies are unnecessary and/or poorly performed. Funding review is required to reflect modern day ultrasound practice ensuring appropriate studies, remuneration that correlates with the type of service and that providers are suitably qualified.

“Funding review is required to reflect modern day ultrasound practice ensuring appropriate studies, remuneration that correlates with the type of service and that providers are suitably qualified. "
DR Matthew Andrews
MBBS (Hons) MMed FRANZCR
Dr Andrews is a radiologist with a special interest in ultrasound and minor interventional procedures. He is immediate Past President of the Royal Australian & New Zealand College of Radiologists (RANZCR), chairs the MIA Victoria Clinical Management Committee, and is Director of Medical Imaging at Cabrini Brighton.
Qualifications:
- FRANZCR (Alfred Hospital)
- MMed (Melbourne University)
- Abdominal Imaging Fellowship (University of California, Davis)
Major Honorary Positions:
- President of RANZCR (2010 & 2011)
- President of Australasian Society of Ultrasound in Medicine ASUM (2006-2008)
- Convenor RANZCR Ultrasound Committee (1995-2009)
- Foundation Member of the RANZCR Standards of Practice and Accreditation Committee
- Principal Councillor for RANZCR Economics & Workforce Portfolio (2007-2010)
National Allied Health Workforce Strategy: a lasting reprieve?
Hospital + Healthcare speaks with Chief Allied Health Officer Anita Hobson-Powell,...
ADHA accelerates connected care for allied health
After attracting substantial interest from software vendors, the Australian Digital Health Agency...
South Australia gains its first fully rural medical degree
Designed to address the critical shortage of doctors in regional, rural and remote areas,...









