Predicting risk of spinal fracture using bioengineering

The World Health Organization has recently named the next ten years as the “decade of healthy ageing”.
But the global COVID-19 pandemic may hamper this goal, as reduced movement due to social distancing has the potential to negatively impact our physical fitness, leading to severe muscle and bone diseases.
One of the biggest health issues during ageing is osteoporosis, named a “silent bone disease” since there are not many symptoms visible to the naked eye.
Bone fracture and its consequences
The human adult skeleton comprises nearly 210 bones that form the foundation of our body. Structural defects, particularly in the spine, can lead to fractures that result in chronic pain, disfigurement, reduced quality of life, and increased risk of dying.
Bone density scanning by dual-energy x-ray absorptiometry (DXA) is routinely used to identify individuals at high risk of bone fracture.
In Australia, the total cost over 10 years of poor skeletal health, mainly due to age-related conditions, is expected to cost around $A 23 billion by 2022. The yearly cost of treating osteoporotic fractures is estimated to be about $US 22 billion in the USA, and this is apart from the societal burdens of such debilitating disease.
Current technologies to detect and predict osteoporosis
Due to often subtle changes in bone structure as a result of osteoporosis – including loss of bone density and the fact that sometimes vertebral fractures can occur without significant symptoms or pain – imaging techniques are used to detect impaired bone strength and diagnose bone fracture.
Most of these techniques are based on X-ray methods to quantify ‘bone mineral density’, a diagnostic tool related to the amount of minerals such as calcium in the bone tissue.
Although these techniques are quite fast, and while they identify individuals at high risk of fracture, there is still room for improvement. Predicting risk of fracture is important to be able to offer patients preventive treatments before fractures occur.
Research has shown that broken bones among older people increase their risk of death by up to 10 years.
A fracture occurs when bone undergoes a mechanical loading or experiences a force that exceeds its strength. However, what mechanical loading is experienced by our bone during daily activities cannot be measured by imaging techniques; this can only be done via invasive intervention such as a sensor inside the body.
Fortunately, there are other ways to achieve this goal using bioengineering principles.
Biomechanical approach to predict osteoporotic vertebral fracture
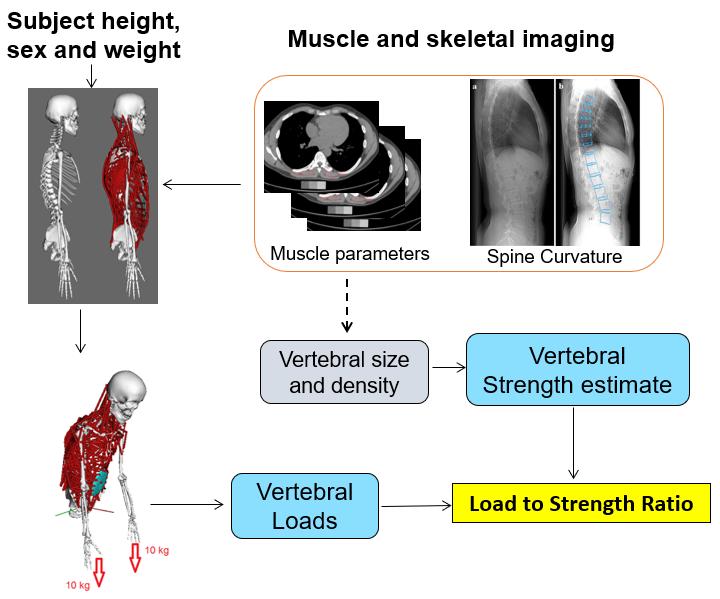
Bone fracture prediction tools require an estimate of both the mechanical loading that the bone experiences and its strength.
To predict spinal loading, our research teams have recently developed computer-based models (biomechanical models) that use a set of mathematical and physics-based representations of human movement so that we can estimate internal loads.
Our models are based on 250 individuals from the Framingham Heart Study cohort.
This is a comprehensive study established in 1948 to identify the risk factors of cardiovascular disease by recruiting over 5209 people (individuals between 30 and 62 years from Framingham, MA, USA) who were deemed to have not yet developed clear symptoms of cardiovascular diseases or experienced stroke or heart attack.
Some of the well-known major risk factors for cardiovascular disease, such as smoking and high cholesterol levels, were first identified in the Framingham cohort after a careful monitoring of its participants over decades. Eventually, data from this study was expanded to investigate other diseases such as dementia, and osteoporosis.
We developed our biomechanical models based on the 3D imaging of vertebrae and trunk muscles of 250 Framingham participants (125 men, 125 women, ages 41 - 90).
We then adjusted every individual’s spinal curvature and muscle morphology to predict internal loading at every single level of the spine during over 100 daily activities including lifting, pushing a shopping cart, tying shoes and shoulder flexion while holding weights.
Next, using spinal imaging, we employed engineering principles to predict vertebral strength at every level (3). Specifically, we estimated the strength based on vertebral size and bone mineral density, as these two factors combined explain the majority of variation in vertebral strength.
As a result, we could predict the load to strength ratio, determined as applied load during an activity divided by strength of each vertebrae for every single person and at each vertebral level (thoracic and lumbar levels). In theory, a load to strength ratio larger than one would indicate that loading exceeds strength, and thus a high risk of vertebral fracture.
What can we learn from biomechanical modelling?
One of the main findings was that we could confirm that the high risk of vertebral fractures in the thoracolumbar region of the spine, located near the bottom of the ribs, corresponds to high load to strength ratios evaluated by our models.
Secondly, our models allowed us to identify the different types of activities that may be associated with an increased risk of fracture in different locations along the spine. The list of daily activities simulated in this study range from neutral standing, to wearing a backpack, pushing a cart and even performing sit-ups.
Specifically, three different spinal regions were identified by a range of activities that generated maximum load to strength ratios: holding a weight in one hand (asymmetrically) for the upper thoracic spine, holding a weight in front of the body for the lower thoracic spine, and flexing forward while lifting or holding a weight for the lumbar spine.
Our results correlated strongly with epidemiological reports of the locations of spinal fractures, also allowing us to show the biomechanical reasons behind these fractures by identifying a range of lifting, asymmetric postures and weight-bearing activities as higher-risk tasks for different regions of the spine.
We believe these findings could open a new avenue toward management of osteoporosis and prevention of osteoporotic vertebral fracture, such as the development of personalised activity recommendations and preventive muscle training since our models can quantify the role of activities and muscles on spinal loading.
The computer models of the spine developed in this study can also be applied in a variety of areas, not only prediction of spinal fractures, but also other spinal conditions including disc herniation, degenerative disc disease, spinal stenosis, spondylosis and neurological disorders, spinal cord injury and even breathing difficulties due to chest muscle malfunctions.
Future direction
Our next step is to determine whether this approach improves the prediction of spine fracture risk compared to currently used methods based on bone density measurements alone.
Our long-term goal is to utilise subject-specific musculoskeletal modelling of the spine to enhance planning of spinal surgical procedures, rehabilitation protocols, preventive training and eventually develop improved predictive tools to avoid this “silent disease” before bone fracture occurs.
Our models are freely available, and include a fully articulated thoracolumbar spine (T1 through L5), with 3 rotational degrees-of-freedom at each inter-vertebral joint, and ribcage.
We acknowledge funding from the National Institutes of Health, National Space Biomedical Research Institute and the US National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services.
This article was first published on Pursuit. Read the original article.

Originally published here.
Stigma around lung disease and cancer must go
Data from Lung Foundation Australia's Lived Experience Survey has showed the debilitating...
High-five for a sustainable path to better hand hygiene
Ahead of World Hand Hygiene Day, an emergency physician explains why hand hygiene is needed all...
Six big ideas for beating brain cancer
The University of Newcastle's Mark Hughes Foundation Centre for Brain Cancer Research has...









