Monash device may reduce risk of artery-widening procedure
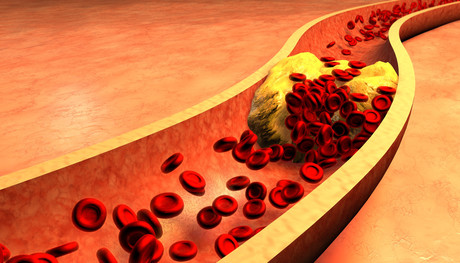
Researchers from Monash University are developing a device to safely and effectively treat the most common cardiovascular disease: atherosclerosis, or narrowing of the arteries. The new device uses balloon angioplasty combined with a light-activated drug coating that may reduce the risk of complications.
Balloon angioplasty — a current treatment for atherosclerosis — involves inflating a small balloon in the affected area of the artery to increase blood flow. Recently, the procedure has involved coating the balloon with paclitaxel — a drug that prevents renarrowing of the vessel — but this has proven to be problematic.
Recent studies suggest that coating the balloon with paclitaxel may cause serious side effects, including toxicity around the region of the balloon up to two years after the procedure. This has prompted the US Food and Drug Administration (FDA) to issue a medical device safety communication.
The Eastern Health Clinical School at Monash University is developing an alternative treatment that uses a light-activated drug to coat the angioplasty balloon and reduce the risk of toxicity.
Associate Professor Anthony Dear said the device, called Lumi-Solve, ensured the drug was targeted to the site of the narrowed artery, and was only activated when exposed to UV light.
“Under the existing angioplasty procedure, when you open a balloon that’s coated with a drug, a lot of it showers off and travels into the blood vessel down the leg, potentially causing reactions away from the intended area,” Assoc Prof Dear said.
“With our system, the drug is not active until the balloon is open and touching the vessel wall at the affected site and then exposed to light, potentially significantly reducing local and systemic toxicity.
“Tens of thousands of people undergo a balloon angioplasty each year, so the benefits of this new technique are potentially enormous.”
Assoc Prof Dear said the procedure may also be safer than treating clogged arteries with stents, as they could cause ongoing health problems.
“As stents are permanent ‘foreign bodies’, they may cause blood clots, which requires patients to take lifelong blood thinners,” Assoc Prof Dear explained.
“And because stents are not flexible they can fracture and rupture the artery wall in some areas of the body, particularly where they cross joints such as hips and knees.”
Assoc Prof Dear said the research team had been working on the new device for several years — well before the FDA communication — and involved scientists from numerous institutes including Bio21 Institute at the University of Melbourne, CSIRO and Baker IDI.
Funded by Monash University and the NHMRC, the Lumi-Solve development program has focused on treating narrowing in leg arteries; however, the new procedure could easily be applied to other areas of the body, including coronary and neck arteries.
View an animation of the procedure here.
Healthscope issues statement on three hospital patient deaths
Healthscope has issued a statement outlining its response to the deaths of three of its...
IVF incident: "All of us at Monash IVF are devastated"
Monash IVF has confirmed that the embryo of one patient at its Brisbane clinic was incorrectly...
NSW sees ramping reductions across some of its busiest EDs
Some of NSW's busiest emergency departments have seen significant reductions in hospital...









